Introduction & Background
This project aims to optimize CRISPR-Cas9 technology for therapeutic use in primary immunodeficiency diseases. The goal is to develop a personalized therapy that can correct patient-specific mutations in autologous harvested stem cells, which will then be given back to the patient.
Primary immunodeficiency diseases can present as infection susceptibility, autoimmune disease, and early cancer. They predominantly affect children. Blood stem cell transplant from a donor can cure most of the conditions, but as the procedure is toxic and potentially lethal, most patients are treated with immunomodulatory drugs.
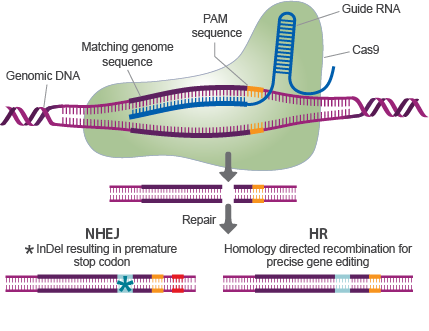
This project develops CRISPR-Cas9 based treatments as an alternative to the bone marrow transplant. CRISPR-Cas involves a Cas nuclease attached to a guide RNA (gRNA) that leads the nuclease to a defined genomic location, which the nuclease then cuts. The cut induces the cellular DNA damage response. The cell can repair the cut either by homology directed repair (HR) or non-homologous end joining (NHEJ) (See Figure 1). Both repair outcomes can be used in primary immunodeficiency therapy. In addition, modifications of the CRISPR-Cas9 system exist; these include Base Editing, Prime Editing, and customized modifications that our laboratory has developed.
Aims of the project
The study has multiple subprojects, and the work will be tailored based on the interests of the student. The Msc student will have a PhD student or postdoc as their hands-on supervisor and will complete their thesis as part of a larger project. Examples of projects include:
- Edit T cells both with conventional and modified CRISPR-Cas9 systems and compare their performance in different diseases
- Edit human blood stem cells, and transplant the edited cells to SCID mouse models
- Screen guides for individual patient mutations
- Set up CRISPR screening methods to identify guides for a large number of patients
- Evaluate CRISPR off-target editing with different Next Generation Sequencing methods
Methods
The projects use a wide variety of methods, including:
- Primary cell culture and transfection
- Cloning, RNA in vitro transcription, PCR, droplet digital PCR
- Next Generation Sequencing library preparation & data analysis
- Work with mouse models
Organization/Collaboration
Our laboratory is 2,5 years old and consists of a medically trained PI, four PhD students (one graduating in 01/2022), three Msc students (two of which will graduate in 01/2022), a lab manager and a postdoc. We are located at the Centre for Molecular Medicine Norway (NCMM), which houses internationally recruited research groups in cutting-edge research infrastructure. The environment is international and the working language is English. We collaborate locally with groups at Oslo University Hospital, as well as complementary research groups in Karolinska Institute (Sweden), Sanger Institute (UK), and University of Helsinki (Finland).
Contact information:
Emma Haapaniemi
+47 41384367
Forskninsgparken
Gaustadallen 21
0349 Oslo
https://www.med.uio.no/ncmm/english/groups/haapaniemi-group/